In 1950, ORINS, the Oak Ridge Institute for Nuclear Studies (now ORAU), opened a 30-bed cancer hospital. It was one of three facilities across the country developed at the urging of the Atomic Energy Commission after the end of World War II and the Manhattan Project to explore the use of radioisotopes in cancer treatment. The other hospitals were located near Argonne National Laboratory in Chicago and Brookhaven National Laboratory in Upton, New York.
In the 24 years during which the ORINS Medical Division cancer hospital admitted patients, 3,500 people were treated. All had been diagnosed with cancer and nearly all of them were considered terminal.
“The ORINS cancer hospital is credited with laying the foundations for nuclear medicine research, pioneering the use of chemotherapy, immunotherapy, teletherapy and brachytherapy, and the development of machines that were precursors to today’s linear accelerators and positive emission tomography scanners,” wrote Michael Holtz, ORAU associate manager, communications and marketing, in his 2023 white paper, Meeting the Moment: Aligning ORAU’s capabilities with the federal government’s priorities to end cancer as we know it (.PDF, 1.9 MB).
Holtz is a 12-year survivor of stage-IIIB rectal cancer. Radiation was part of the protocol he underwent to treat his cancer. Learning about ORAU’s cancer history was a full-circle moment for him.
“We don’t talk about this part of our history very often, but as someone who was treated with radiation it fascinates me that my treatment has its roots here at ORAU,” he said.
The first patient admitted to the cancer hospital was a woman with extensive thyroid cancer. Thyroid cancer became an early focus of the ORINS Medical Division’s work.
Early work treating thyroid cancer
Marshall Brucer, M.D., the first director of the ORINS Medical Division, developed 9 thyroid phantoms, devices that simulated the human neck and thyroid and were used for equipment calibration in thyroid uptake studies. These studies were crucial in evaluating thyroid function. The thyroid phantoms Brucer developed were created from department store mannequins named “Abigail, Bridget, Chloe, Drucilla, Euphemia and so on through Rhoda with a special one for a difference purpose named Anne Boleyn.” These mannequins, which contained approximately a metal Dixie-cup’s worth of mock iodine in artificial thyroid glands that were inserted in their necks, were sent around the world to train medical personnel in their use for equipment calibration.
That mock iodine referenced above was developed by the medical division team in 1954-55. Radioactive iodine, or iodine-131, has long been used to detect and diagnose thyroid cancer but has an extremely short half-life of just eight days. The ORINS medical team created a carefully proportional mixture of barium-133 and cesium-137, which gave nearly the same gamma spectrum appearance as iodine-131. Its longer half-life made it an ideal source for calibrating thyroid uptake machines before they were used on patients.
Development of radiotherapy machines
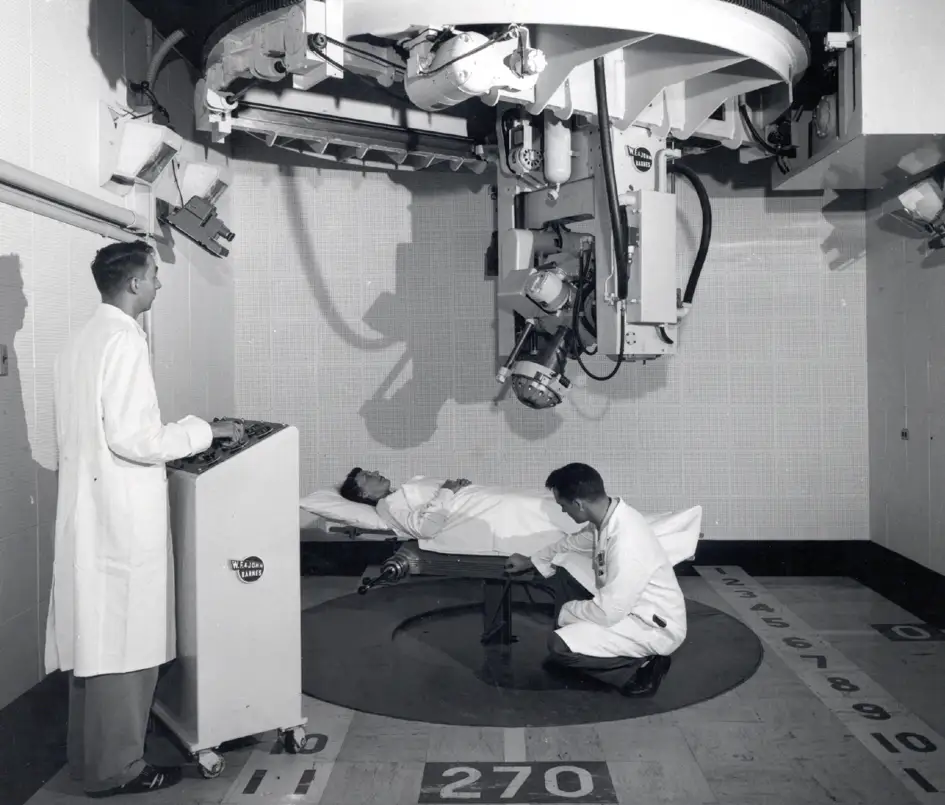
Members of the ORINS medical team were involved in the development of several radiotherapy treatment machines. In one case, Brucer and team participated in a cooperative project with M.D. Anderson Cancer Center to develop an efficient Cobalt-60 teletherapy machine. Space had to be specially built at ORINS for the device. After testing at ORINS, the device was moved to M.D. Anderson for clinical trials.
Another example of ORINS medical professionals developing a cutting-edge cancer radiation treatment device was the development of an early linear scanner. In collaboration with Oak Ridge National Laboratory, scientists worked to improve the resolution of two-dimensional maps of the human body that were produced by a “radiation head on a cantilevered arm which moves back and forth over a patient.” This scanning device was used to determine how radioisotopes were distributed and how they behaved in patients receiving diagnostic or therapeutic doses of radioisotopes. The linear scanner was first introduced at the University of California, but the improvements made during testing by the Oak Ridge team were incorporated in commercial models developed for cancer treatment centers around the country.
Advances in cancer treatment
The ORINS Medical Division was on the forefront of many advances in cancer treatment, including but not limited to the following:
- Advancement of bone marrow transplantation. ORINS’ Gould Andrews, M.D., studied the effectiveness of bone marrow transplantation in the treatment of victims of radiation accidents.
- Development of gallium-67 as a radiopharmaceutical. ORINS medical staff first developed gallium-67 as a scanning agent for locating soft-tissue tumors. Then, in the early 80s, ORAU staff determined how it could be used in a diagnostic procedure for finding postoperative infections. Gallium-67 has wide use in nuclear medicine to this day.
- Development of carbon-11-labeled amino acids as radiopharmaceuticals. ORAU staff synthesized and purified carbon-11-labeled amino acids for use in positron emission computerized tomography (what we call PET scans today). These amino acids could be used for differential diagnosis of pancreatic diseases and detection of solid tumors.
- Development of cobalt teletherapy. Brucer was a major contributor to the development of teletherapy using cobalt-60. Cobalt-60 became the most widely used teletherapy source across the world.
- Development of cesium teletherapy. Brucer was also a key contributor to the development of cesium teletherapy, in which cesium was used in place of cobalt.
- Creation of cesium teletherapy machines. Brucer helped develop machines like the 1540 curie cesium-137 unit, which targeted diseased tissue and reduced impact on healthy tissue. Leonard G. Grimmett, Ph.D., at MD Anderson Cancer Center in Houston was co-develop.
- Development of total body irradiation. Brucer and Andrews developed an approach for delivering a uniform whole-body dose of radiation and used it to treat some forms of cancer, particularly leukemia and lymphoma. Employing whole body irradiation with significantly higher doses than those used at ORAU became established medical practice for treatment of blood and other cancers.
Pioneering nuclear medicine
In addition to these important advancements in cancer treatment, the ORINS Cancer Hospital was a pioneer in the field of nuclear medicine. The treatment advancements were remarkable, to be certain, and the hospital also created the early workforce for this new field of medicine. In addition to Drs. Brucer and Andrews, other medical professionals who worked at the forefront of this emerging field included Frank Comas, M.D., Ph.D., radiation therapist; Ralph Kniseley, M.D.; George LeRoy, M.D., who led studies of lanthanum as part of tracer studies for gastrointestinal absorption; Clarence Lushbaugh, Ph.D., who lead the Total Body Irradiation program; Karl Hubner, M.D., hematologist; Ray Hayes, Ph.D., who led the development of radionuclides and radiopharmacy; Fred Snyder, Ph.D., who was in the lipid program; Helen Vodopick, M.D., Frank Goswitz, M.D., Nazareth Gengozian, Ph.D., who developed experiments for use in immunology; Lowell Edwards, M.D. chief clinical investigator; and the many nurses, technologists and other personnel who were required for the operation of the hospital.
The cancer hospital was closed in 1974 after the U.S. Department of Energy determined that the fields of nuclear medicine, oncology, and others were thriving in world outside of the government department. The Medical Division continued work well into the 1990s, including research on cotton-top tamarins, the only other mammal besides human beings that spontaneously develops colorectal cancer.
When the cancer hospital closed, many of the doctors on staff envisioned the establishment of the Radiation Emergency Assistance Center/Training Site (REACTS), which would provide 12 emergency response and subject matter expertise on the medical management of radiation incidents. REAC/TS was established in 1975 and moved to its current location on the campus of Methodist Medical Center in Oak Ridge. Today, REAC/TS is a world renowned U.S. Department of Energy (DOE) asset, situated under DOE’s Oak Ridge Institute for Science and Education (ORISE), which is managed by ORAU.
While neither the research hospital nor the Medical Division exists today, ORAU has built on its legacy by continuing to demonstrate its capabilities in the cancer space. These capabilities include epidemiology and exposure science, peer review and health communications.